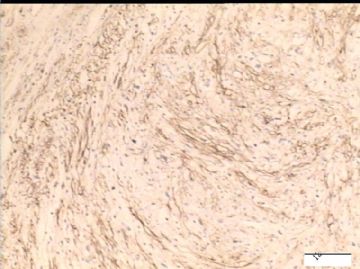
| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
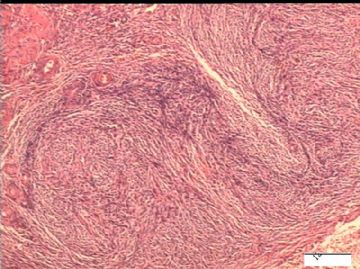
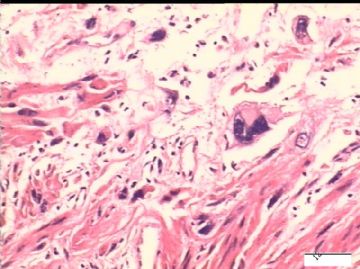
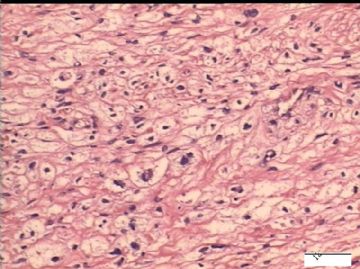
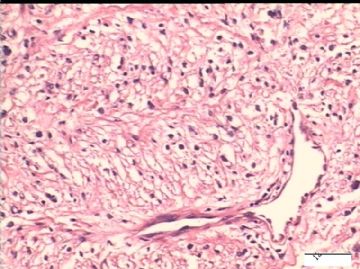
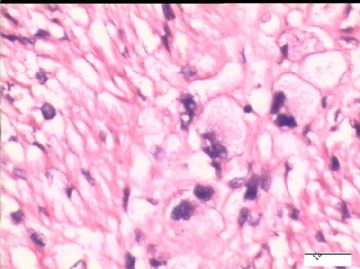
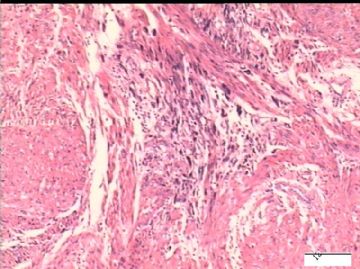
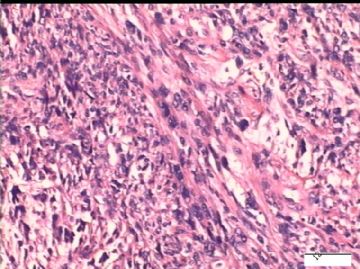
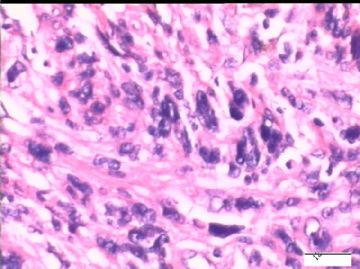
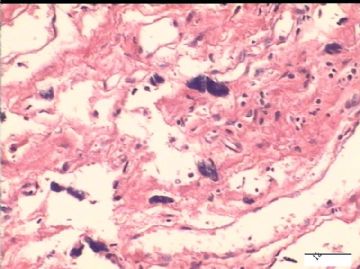
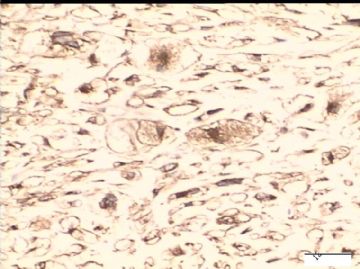
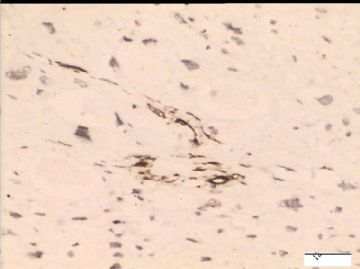
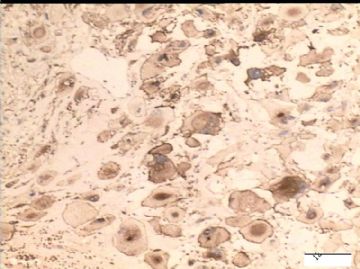
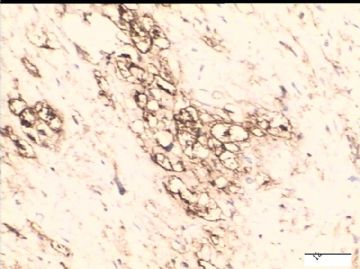
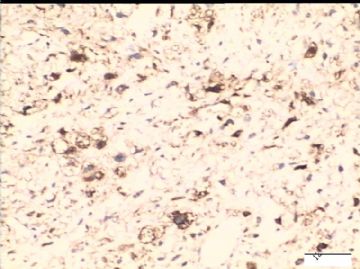
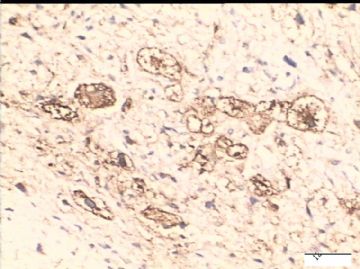
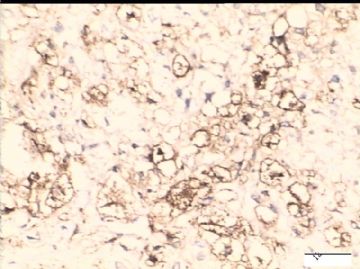
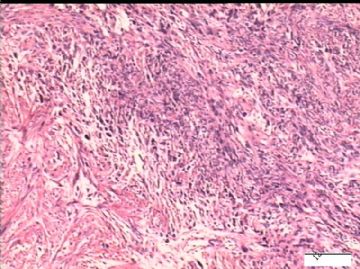
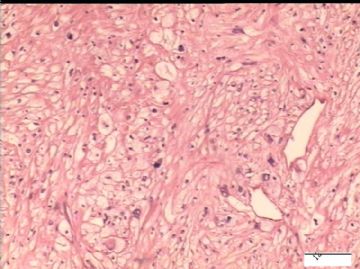
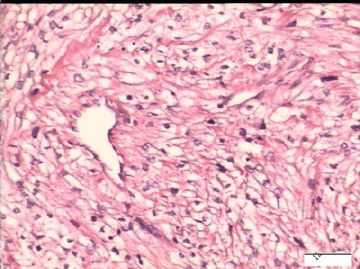
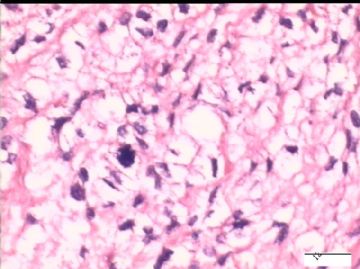
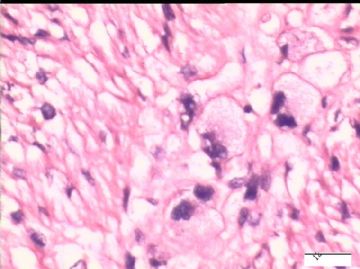
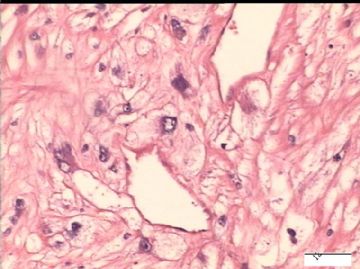
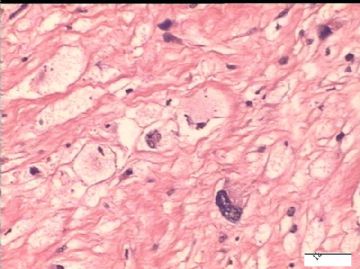
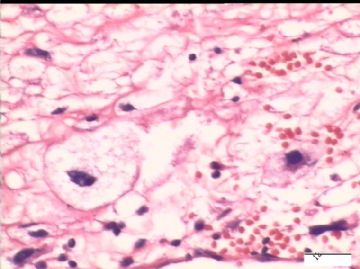
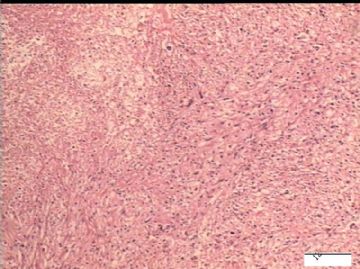
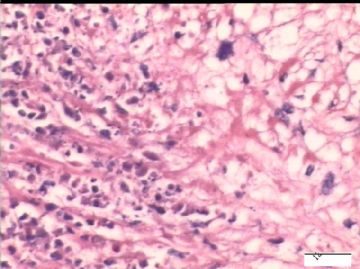
- 51岁/子宫肿瘤
| 以下是引用xljin8在2010-1-27 20:06:00的发言: 病理诊断“子宫PEComa ”有不同意见吗? |
组织学图象也符合
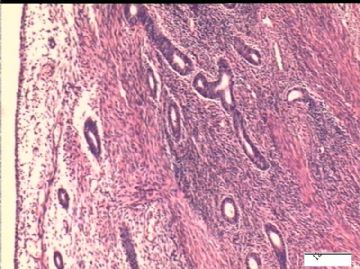
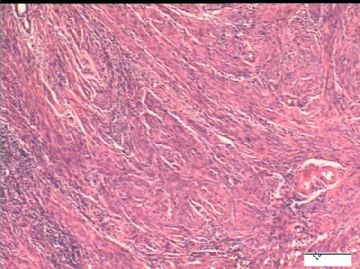
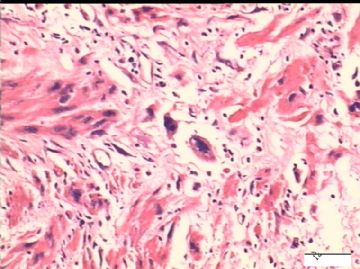
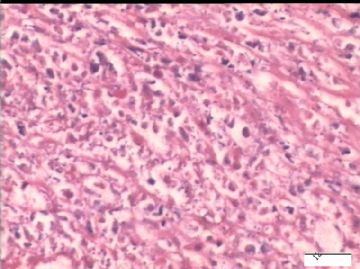
PEComas具有以下两个或更多特征时要考虑恶性的或者高危侵袭行为,直径> 5 cm,边缘浸润,瘤细胞坏死,核分裂象> 1个/50 HPF,脉管侵犯,高级别的核或胞质。
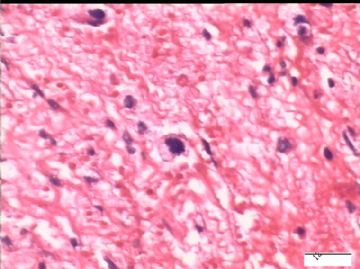
PEComas具有多形性核或者多核巨细胞之一或者体积> 5 cm都被考虑为不确定潜在恶性。
PEComas体积< 5 cm,低级别细胞学,核分裂象(< 1个/50HPF),没有浸润,没有坏死或者血管浸润都被考虑为临床良性的。
-
本帖最后由 于 2010-01-28 04:38:00 编辑
Agree with the interpretation from Dr. Zhang.
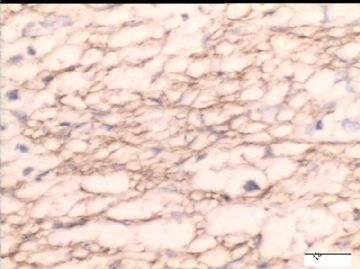
I would like to see the IHC results.
If smooth muscle markers and HMB45 or melan A or s100 positive, it is a PEComa.
If only smooth muscle markers pos, it is leiomyosarcoma (atypia + tumor necrosis or mitoses).
Am J Surg Pathol. 2005 Dec;29(12):1558-75.
Perivascular epithelioid cell neoplasms of soft tissue and gynecologic origin: a clinicopathologic study of 26 cases and review of the literature.
Folpe AL, Mentzel T, Lehr HA, Fisher C, Balzer BL, Weiss SW.
Department of Pathology and Laboratory Medicine, Emory University, Atlanta, GA 30322, USA. afolpe@emory.edu
PEComas, occasionally associated with the tuberous sclerosis complex, are defined by the presence of perivascular epithelioid cells that coexpress muscle and melanocytic markers. This family of tumors includes angiomyolipoma (AML), clear cell sugar tumor of the lung (CCST), lymphangioleiomyomatosis (LAM), and very rare tumors in other locations. Because non-AML/non-LAM PEComas are extremely rare and their natural history and prognostic features undefined, we present our experience with 26 PEComas of soft tissue and the gynecologic tract, the largest series to date. We also performed a detailed review of the literature, with special attention to features predictive of clinical behavior. All PEComas exclusive of AML and LAM were retrieved from our consultation files. Immunohistochemistry for pan-cytokeratin (CK), S-100 protein, smooth muscle actins (SMA), desmin, vimentin, HMB45, Melan-A, microphthalmia transcription factor (MiTF), TFE3, CD117, and CD34 was performed. Clinical follow-up information was obtained. Fisher's exact test was performed. The median patient age was 46 years (range, 15-97 years); there was a marked female predominance (22 females, 4 males). Sites of involvement included the omentum or mesentery (6 cases), uterus (4 cases), pelvic soft tissues (3 cases), abdominal wall (2 cases), uterine cervix (2 cases), and vagina, retroperitoneum, thigh, falciform ligament, scalp, broad ligament, forearm, shoulder, and neck (1 case each). The tumors ranged from 1.6 to 29 cm in size (median, 7.8 cm). Tumors were epithelioid (N = 9), spindled (N = 7), or mixed (N = 10). Multinucleated giant cells were present in 18 cases. High nuclear grade was noted in 10 cases, high cellularity in 7 cases, necrosis in 8 cases, and vascular invasion in 3 cases. Mitotic activity was 0 to 50 mitotic figures (MF)/50 high power fields (HPF) (median, 0 MF/50 HPF) with atypical MF in 6 cases. IHC results were: SMA (20/25), desmin (8/22), HMB45 (22/24), Melan-A (13/18), MITF (9/18), S-100 protein (8/24), CK (3/23), vimentin (12/14), TFE3 (5/17), c-kit (1/20), and CD34 (0/7). Clinical follow-up (24 of 26 patients, 92%; median, 30 months; range, 10-84 months) showed 3 local recurrences and 5 distant metastases. At last available clinical follow-up, 2 patients (8%) were dead of disease, 4 patients (17%) were alive with metastatic or unresectable local disease, and 18 patients (75%) were alive with no evidence of disease. No patient in our series had a history of tuberous sclerosis complex. Recurrence and/or metastasis was strongly associated tumor size > median size (8 cm), mitotic activity greater than 1/50 HPF, and necrosis. We conclude that PEComas of soft tissue and gynecologic origin may be classified as "benign," "of uncertain malignant potential," or "malignant." Small PEComas without any worrisome histologic features are most likely benign. PEComas with nuclear pleomorphism alone ("symplastic") and large PEComas without other worrisome features have uncertain malignant potential. PEComas with two or more worrisome histologic features should be considered malignant. Occasional PEComas express unusual markers, such as S-100 protein, desmin, and rarely CK. The role of TFE3 in PEComas should be further studied.
Based on IHC results (smooth muscle marker pos and HMB45 pos) and the morphology (marked atypia, necorosism mitosis), large size (10 cm), it is malignant PEComa.
Not sure the treatment for uterine PEComa. I think it may be similar to uterine leiomyosarcoma.